Hysteroscopy at TFI: A Clearer Path to Fertility
When trying to grow your family, understanding the root causes of infertility or miscarriage is essential. At Tennessee Fertility Institute (TFI), one of the most powerful tools we use to evaluate and treat uterine conditions is hysteroscopy—a minimally invasive procedure that offers both clarity and solutions.
What Is Hysteroscopy?
Hysteroscopy allows fertility specialists to directly view the inside of the uterus using a slim, lighted device called a hysteroscope. Inserted through the cervix, this tool provides real-time visuals of the uterine cavity. The procedure can be:
-
Diagnostic: Used to observe and assess the uterine environment.
-
Operative: Used to treat abnormalities found during the diagnostic phase.
Unlike ultrasound or HSG imaging, hysteroscopy offers a direct, unobstructed view—making it ideal for identifying and addressing issues that may interfere with conception.
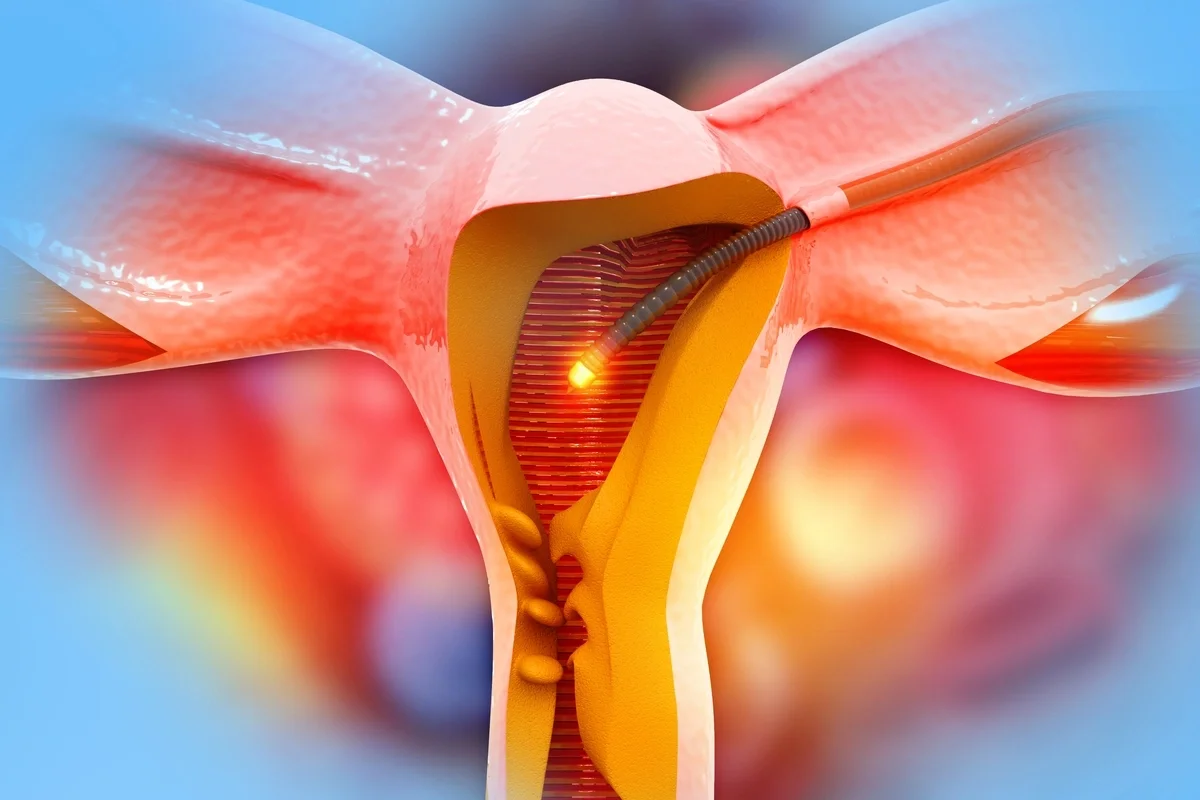
Illustration of hysteroscope
Why Might Hysteroscopy Be Recommended?
At TFI, hysteroscopy is often part of a comprehensive fertility evaluation, especially for patients experiencing:
Recurrent Pregnancy Loss (RPL)
Patients with two or more miscarriages often undergo hysteroscopy to identify structural abnormalities like a uterine septum, fibroids, or adhesions. Hysteroscopy enables precise resection of these anomalies, restoring a more favorable environment for embryo implantation and gestation.
Unexplained Infertility
When standard evaluations fail to reveal a cause, hysteroscopy can uncover subtle intrauterine issues missed by ultrasound or HSG. These may include a thin endometrium, polyps, or minor adhesions that impair implantation. By treating these findings, hysteroscopy enhances uterine receptivity and increases the likelihood of spontaneous or assisted conception.
Failed IVF Cycles
Repeated IVF failures often prompt a reevaluation of the uterine cavity. Hysteroscopy is considered the gold standard for this purpose. It allows clinicians to identify and correct abnormalities that may have interfered with previous embryo transfers. Research shows that patients who undergo hysteroscopy before IVF have higher pregnancy rates and lower miscarriage rates compared to those who do not.
Irregular Bleeding or Suspected Uterine Abnormalities
Abnormal bleeding may signal the presence of fibroids, polyps, or endometrial hyperplasia. Hysteroscopy provides a direct view of the uterine lining and facilitates targeted biopsy or removal of lesions. This not only resolves symptoms but also improves fertility outcomes by restoring normal endometrial function.
Preparation for Embryo Transfer
Before embryo transfer—especially in frozen cycles—hysteroscopy ensures the uterine cavity is free of obstructions and optimally prepared for implantation. Timing the procedure within 2–6 months of transfer is ideal for maximizing success.
What to Expect at TFI
At TFI, most hysteroscopies are performed in-office and the duration depends on whether the procedure is diagnostic (to examine the uterus) or operative (to treat a condition). Here’s a step-by-step look at what patients can expect:
Before the Procedure
-
Timing: Hysteroscopy is usually scheduled between days 5 and 12 of the menstrual cycle, when the uterine lining is thinnest and visibility is optimal. Patients can also use birth control pills to keep their lining thin, allowing for more flexible scheduling and timing.
-
Preparation: Patients may be asked to avoid tampons, douching, and/or intercourse for 24 hours prior to the procedure.
-
Medication: In some cases, a medication may be prescribed to soften or dilate the cervix, making insertion of the hysteroscope easier.
-
Anesthesia: Most in-office procedures use local anesthesia or light sedation, though general anesthesia may be used for more complex operative hysteroscopies.
During the Procedure
-
Positioning: Patients lie on an exam table similar to a pelvic exam setup.
-
Insertion: A thin, lighted tube called a hysteroscope is gently inserted through the vagina and cervix into the uterus.
-
Visualization: The uterine cavity is expanded using saline, which helps clear mucus and blood and allows for a clear view of the uterine lining.
-
Diagnosis or Treatment: If abnormalities like polyps, fibroids, or adhesions are found, they may be removed immediately using specialized instruments passed through the hysteroscope. This avoids the need for a second procedure.
After the Procedure
-
Recovery Time: Most patients experience mild cramping or spotting for a day or two. These symptoms are typically short-lived and manageable with over-the-counter pain relief.
-
Activity: Patients can usually resume normal activities within 24 hours, though it’s advised to avoid intercourse, tampon use, and/or strenuous exercise for a few days.
-
Follow-Up: If tissue was removed or biopsied, results are typically reviewed during a follow-up visit. Patients are encouraged to report any unusual symptoms such as heavy bleeding, fever, or severe pain.
Why Choose TFI?
At TFI, we combine advanced technology with compassionate care. Our team uses hysteroscopy not just to diagnose, but to actively improve fertility outcomes. Whether you’re just beginning your journey or preparing for IVF, hysteroscopy may be the key to unlocking your path forward.
Ready to learn more? Schedule a consultation with our team to see if hysteroscopy is right for you. At TFI, we’re here to help you move forward—with answers, support, and expert care.