An Introduction to Mosaic Embryos
Advances in preimplantation genetic testing (PGT) have made it possible to identify embryos with chromosomal variations, including mosaic embryos. If you’ve recently received a mosaic embryo report, you may feel uncertain or even anxious. Mosaicism is a nuanced topic, and understanding what it means—and what questions to ask—can help you make informed decisions.
What Is a Mosaic Embryo?
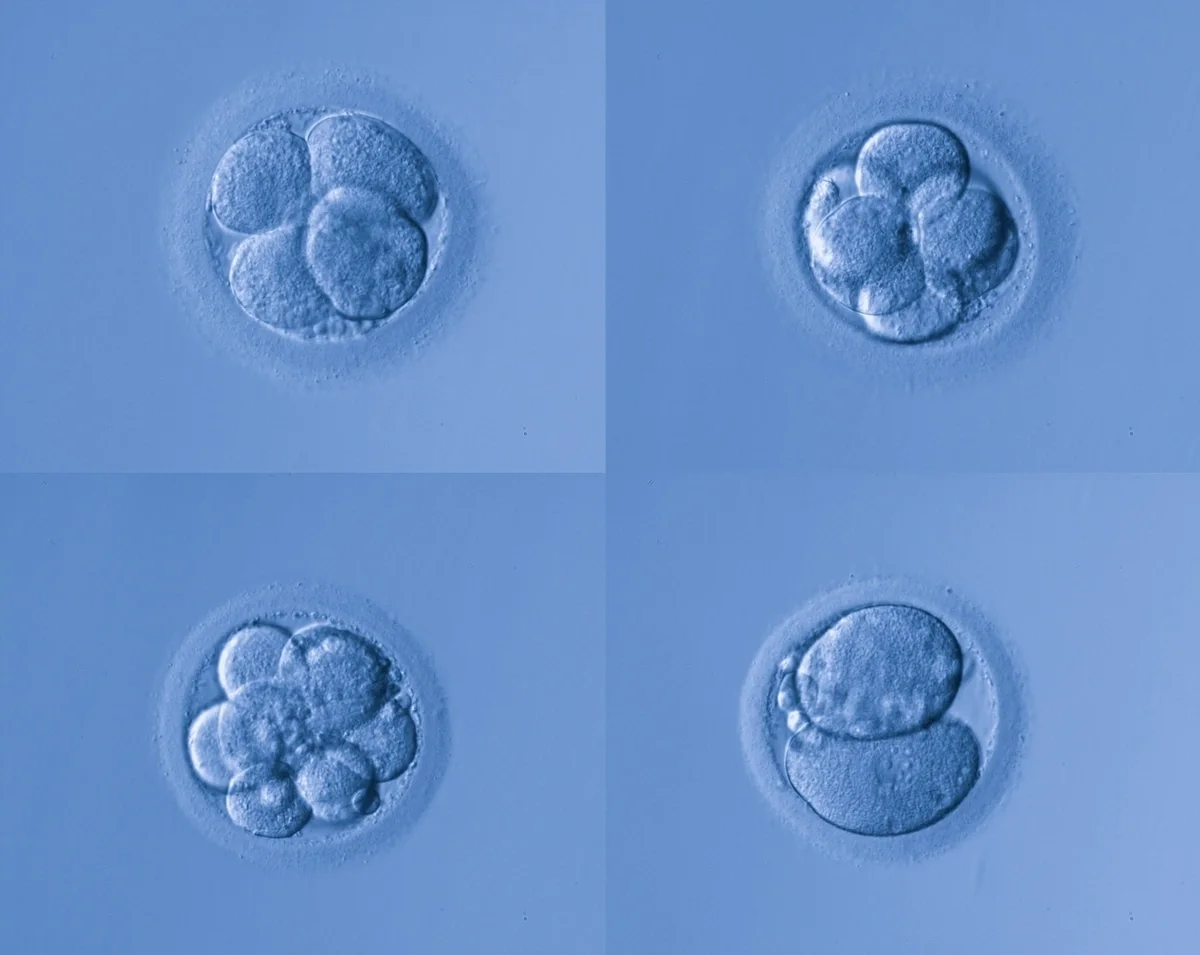
A mosaic embryo contains a mix of chromosomally normal (euploid) and abnormal (aneuploid) cells. This occurs when errors in chromosome division happen early in development. Importantly, mosaicism is not caused by anything you did during treatment.
Because PGT-A analyzes cells from the trophectoderm (the layer that becomes the placenta), the biopsy may not fully represent the inner cell mass (which becomes the fetus). This means the test provides a snapshot—not a complete picture—of the embryo’s chromosomal makeup.
Mosaicism is common, with some studies suggesting that it occurs in 5–20% of embryos tested with PGT-A. It’s also important to note that a mosaic embryo does not automatically mean that embryo will have birth defects. Many mosaic embryos result in healthy pregnancies.
Classifications of Mosaic Embryos
Mosaic embryos are typically categorized by:
-
Type of Chromosomal Change:
-
Mosaic monosomy: One copy of a chromosome instead of two.
-
Mosaic trisomy: Three copies of a chromosome instead of two.
-
-
Level of Mosaicism:
-
Low-level: Usually <30% abnormal cells.
-
High-level: Often >50% abnormal cells.
-
-
Chromosome Involved: Certain chromosomes are associated with higher risks of implantation failure or specific syndromes.
Professional groups like the Preimplantation Genetic Diagnosis International Society (PGDIS) have published prioritization guidelines, but these are evolving and should be interpreted with your provider.
Making Decisions, Understanding Risks, and Why Counseling Matters
When a mosaic embryo is identified, your care team will typically rank embryos for transfer priority based on factors like level of mosaicism and chromosome type. While euploid embryos are generally preferred, mosaic embryos can still result in healthy pregnancies. However, success rates may be lower compared to fully normal embryos, and there is a slightly increased risk of miscarriage or complications such as placental abnormalities. In rare cases, certain chromosomal patterns may be linked to syndromes, which is why individualized counseling is essential.
If you choose to transfer a mosaic embryo, your provider may recommend additional prenatal testing to confirm the baby’s chromosomal health. These steps are not meant to alarm but to provide reassurance and clarity. It’s important to remember that most babies born from mosaic embryos are chromosomally normal, but because no single biopsy can fully represent the entire embryo, uncertainty remains.
Ultimately, the decision to transfer a mosaic embryo should be made in partnership with your physician and genetic counselor. They can help you weigh the potential benefits and risks in the context of your age, embryo quality, and personal goals. There is no universal “right” answer—only what aligns best with your circumstances and family-building journey.
Final Thoughts
It’s important to keep in mind that mosaic embryos are not inherently “bad” or “good”—they represent a spectrum of possibilities. The risks and success rates do vary by chromosome, level of mosaicism, and individual patient factors, and it’s essential to have open, informed conversations with your care team before making any decision.
If you’ve received a mosaic embryo report, schedule a consultation with your provider to review your options and discuss what’s best for your family-building journey.

