Intrauterine Insemination (IUI): 10 Common Questions, Answered
If you’re just starting your fertility journey, you’re likely navigating a sea of acronyms, terms, and treatment options. One of the most common fertility treatments—and often one of the first recommended—is intrauterine insemination (IUI).
At Tennessee Fertility Institute (TFI), we’re here to make fertility care as understandable and approachable as possible. Here are 10 common questions we hear about IUI, along with clear, compassionate answers to help you feel informed and empowered.
1. What is intrauterine insemination (IUI)?
Intrauterine insemination (IUI) is a fertility treatment that involves placing sperm directly into a woman’s uterus during ovulation to increase the chances of fertilization.
By bypassing the cervix and placing sperm closer to the egg, IUI improves the likelihood that the sperm will reach and fertilize the egg—especially helpful in cases where sperm count or motility is a concern.
2. Who is a good candidate for IUI?
IUI is often recommended as a first-line treatment in cases where simpler interventions have not worked or when timing and sperm quality need a boost. It can be especially helpful in the following situations:
-
Mild male factor infertility: If sperm count, motility (movement), or morphology (shape) is slightly below normal, IUI can help by concentrating and placing the healthiest sperm directly into the uterus, giving them a better chance of reaching the egg.
-
Unexplained infertility: When standard testing doesn’t identify a clear cause, IUI—especially when combined with ovulation-inducing medications—can improve timing and increase the odds of fertilization.
-
Cervical factor infertility: Sometimes, cervical mucus is too thick or acidic, making it difficult for sperm to pass through the cervix. IUI bypasses the cervix entirely, placing sperm directly into the uterus.
-
Ovulatory disorders: For patients who ovulate irregularly or not at all, medications can be used to stimulate ovulation, and IUI can help ensure sperm are present at the optimal time.
-
Sexual dysfunction or timing issues: IUI may help when intercourse is infrequent or difficult due to physical, psychological, or logistical challenges.
-
Donor sperm use: IUI is the most common method for insemination when using donor sperm—for single parents by choice, same-sex couples, or couples with severe male factor infertility.
Because it’s relatively quick, minimally invasive, and lower cost than IVF, IUI is often the first treatment step before considering more advanced options. Your provider will work with you to determine if IUI fits your diagnosis, goals, and timeline.
3. How does IUI actually work?
The IUI process involves a series of carefully timed steps that are designed to give sperm the best possible chance of reaching and fertilizing an egg. Here’s a breakdown of what typically happens during an IUI cycle:
-
Cycle Monitoring: Your provider will monitor your menstrual cycle closely using bloodwork and transvaginal ultrasounds. These tests help track the growth of follicles (which contain eggs) and measure hormone levels, especially estrogen and luteinizing hormone (LH).
-
Ovulation Timing: Once a mature follicle is detected, ovulation is timed precisely. This can happen naturally, or your provider may prescribe a "trigger shot" (hCG injection) to ensure the egg is released at the optimal time. IUI is usually scheduled about 24-36 hours after ovulation is confirmed or induced.
-
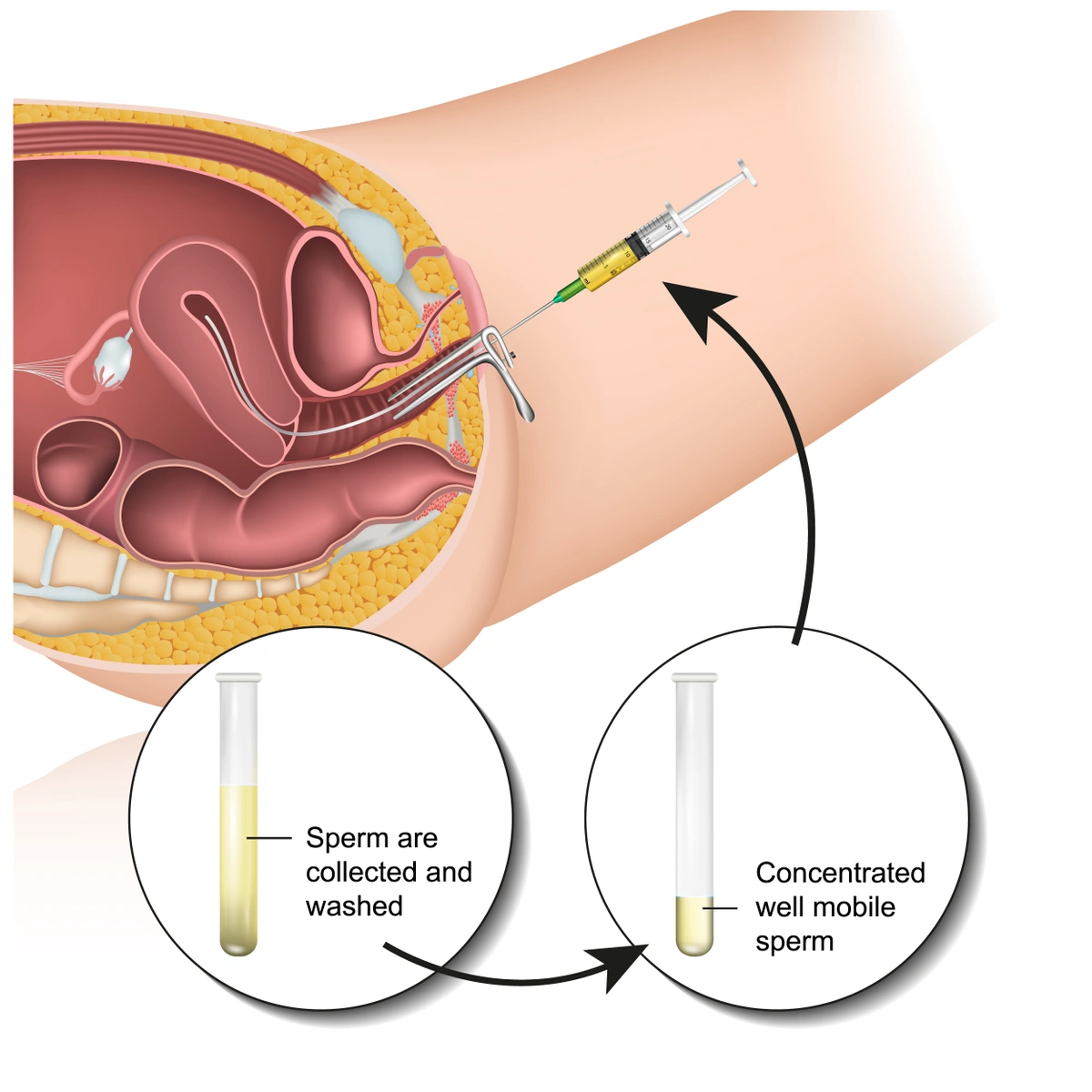
Sperm Sample Preparation: A sperm sample is collected from your partner or a donor. To maximize sperm quality, patients are usually advised to abstain from ejaculation for 2–5 days before the sample is given. The sample is then “washed” in the lab to remove seminal fluid and isolate the healthiest, most motile sperm. This concentration process improves the chances of fertilization and reduces discomfort during the procedure.
-
Insemination Procedure: During the procedure, you’ll lie on an exam table similar to a Pap smear. A speculum is inserted into the vagina, and a thin, flexible catheter is used to insert the prepared sperm directly into the uterus. The process takes just a few minutes and is typically painless, though some patients may feel slight cramping or pressure.
-
Post-Procedure & Next Steps: You may rest briefly after the procedure, then return to normal activity the same day. Two weeks later, you’ll take a pregnancy test to determine if the cycle was successful. This waiting period—often referred to as the "two-week wait"—can be emotionally intense, so it’s a great time to lean on support systems and practice self-care.
Illustration of insemination procedure
4. What role do medications play in IUI cycles?
IUI can be done with or without fertility medications. In many cases, we use medications like:
-
Clomiphene citrate (Clomid) or letrozole (Femara) to induce ovulation
-
Gonadotropins to stimulate the ovaries to produce more than one egg
These medications increase the chances of a successful cycle but may also increase the risk of multiples (twins or more). Your provider will help determine the best medication protocol for your body and goals.
5. What are the success rates for IUI?
Success rates for IUI vary depending on age, diagnosis, and whether medications are used. On average:
-
Women under 35 have a 10–20% chance of pregnancy per cycle
-
Women 35–40 may see success rates of 10–15%
-
Over age 40, rates tend to decline
Success is also cumulative—many patients conceive within 3–4 IUI cycles. If IUI isn’t successful after several attempts, your provider may recommend transitioning to in vitro fertilization (IVF) or another treatment path.
6. What’s the difference between IUI and IVF?
IUI and IVF are both fertility treatments, but they differ significantly in terms of complexity, cost, and success rates. Here's how they compare:
-
IUI (Intrauterine Insemination) is a simpler, less invasive procedure where washed sperm is placed directly into the uterus around the time of ovulation. Fertilization happens naturally inside the body.
-
Who it’s for: IUI is often recommended for those with mild male factor infertility, ovulatory disorders, unexplained infertility, or for individuals/couples using donor sperm.
-
Timeline: One IUI cycle typically spans 2–3 weeks.
-
Cost: IUI is significantly less expensive than IVF and may be partially or fully covered by insurance, depending on your plan. The self-pay or out of pocket cost of an IUI cycle starts at $2,500. Please check out our fertility costs for the most up-to-date service pricing.
-
Success rates: Success per cycle can range from 10–20%, depending on age and underlying conditions.
-
-
IVF (In Vitro Fertilization) involves stimulating the ovaries to produce multiple eggs, retrieving the eggs, fertilizing them in a lab, and then transferring one or more embryos into the uterus.
-
Who it’s for: IVF may be recommended when IUI hasn’t been successful, or in cases of blocked fallopian tubes, diminished ovarian reserve, advanced maternal age, severe male factor infertility, or when using donor eggs or a gestational carrier.
-
Timeline: IVF cycles typically last 4–6 weeks, plus additional time for embryo testing or freezing, if needed.
-
Cost: IVF is more costly than IUI, though financial assistance and insurance benefits may be available. The self-pay or out of pocket cost of an IVF cycle starts at $12,950. Please check out our fertility costs for the most up-to-date service pricing.
-
Success rates: IVF offers higher success rates per cycle than IUI—especially for patients under 40—and can also provide more control over timing and embryo selection. You can view our 2023 SART Clinic Data here.
-
Both treatments have their place in fertility care. Your TFI provider will help determine which path makes the most sense based on your diagnosis, personal preferences, and family-building goals.
7. What are the risks of IUI?
IUI is generally safe, but like all medical procedures, it carries some risks:
-
Mild cramping or spotting after the procedure
-
A very small risk of infection
-
Increased risk of multiple pregnancy (twins or more) when ovulation-stimulating medications are used
Your TFI provider will monitor you closely to reduce risks and adjust treatment if needed.
8. How should I prepare for an IUI cycle?
Leading up to your IUI, you may be asked to:
-
Track ovulation with at-home kits or in-office testing
-
Avoid certain medications or supplements
-
Abstain from sex or ejaculation for 2–5 days before the sperm sample is collected to ensure optimal sperm count
You’ll also have regular appointments to monitor your cycle, so flexibility in your schedule can be helpful.
9. How much does IUI cost?
IUI is typically one of the most affordable fertility treatments, especially compared to IVF. Costs can vary based on whether medications are used and how much monitoring is required.
At Tennessee Fertility Institute, the self-pay or out of pocket cost of an IUI cycle starts at $2,500 and is inclusive of ultrasounds, sperm washing, and insemination.
Some insurance plans may cover diagnostic testing and IUI treatment. Our financial counselors are here to help you understand your coverage, estimate out-of-pocket costs, and explore financing options if needed.
10. What happens after the IUI procedure?
After insemination, you’ll go about your normal routine. There’s no required downtime, though we recommend taking it easy for the rest of the day.
You’ll return to the clinic in about two weeks for a pregnancy test. Waiting during this “two-week wait” can be emotionally challenging, and we encourage self-care and support during this time.
Still have questions? We’re here to help!
If you think IUI might be right for you—or you’re just beginning to explore your options—schedule a consultation with our team at Tennessee Fertility Institute. We’ll walk you through every step and provide the compassionate, personalized care you deserve!